DETAILED HELICOBACTER PYLORI FACT SHEET
The inside of the stomach is bathed in about half a gallon of gastric juice every day. Gastric juice is composed of digestive enzymes and concentrated hydrochloric acid, which can readily tear apart the toughest food or microorganism. Bacteria, viruses, and yesterday’s steak dinner are all consumed in this deadly bath of chemicals. It used to be thought that the stomach contained no bacteria and was actually sterile, but the bacteria Helicobacter pylori changed that. Normally the high acid concentration in the digestive tract prevents bacteria from surviving in this environment. H. pylori, however, lives in the digestive tract lining where it is protected from the body’s defense system. The inflammation (swelling, pain, redness, and warmth) of the tissues caused by H. pylori contributes to a breakdown of the lining with this breakdown eventually producing an ulcer. The details of these bacteria, the damage it causes and how it is being controlled are discussed below.
What are Helicobacter Pylori?
Helicobacter pylori are a type of gram-negative bacteria, spiral in shape with sheathed flagella that researchers now believe are the main cause of peptic ulcers. They thrive in highly acidic environments and are found in the gastric mucous layer or adherent to the epithelial lining of the stomach. Helicobacter pylori have a unique way of adapting in the harsh environment of the stomach. They are microaerophilic, intestinal bacteria that cause the majority of ulcers in the stomach and duodenum.
Helicobacter pylori (H. pylori) have been classified as Class I carcinogens by the World Health Organization and in spite of the widespread occurrence of the diseases attributable to the organisms, little is known about their mode of transmission and microbial ecology.
The History of Helicobacter Pylori and Ulcers
Although Helicobacter pylori are now commonly associated with being one of the main causes of ulcers, this was not always the case. Before 1982 when the bacterium had not yet been discovered, ulcers were commonly associated with stress, acid, eating spicy food and an unhealthy lifestyle. The ulcers were treated by prescribing long-term medications that would treat and lessen the symptoms and perhaps heal the ulcer, but would not cure the infection. When the medications were no longer taken, the ulcers would come back.
Once it was discovered that the majority of ulcers were linked with a bacterial infection, the proper medications could be recommended to eliminate the infection with a small chance of the ulcers returning. It was determined that a one or two week course of antibiotics would cure ulcers caused by H. pylori, and that stress and an unhealthy diet may irritate the ulcer, but would not cause it.
The Life Cycle (Pathogenesis) of Helicobacter Pylori
H. pylori are able to survive in stomach acid because they secrete enzymes that neutralize the acid. This process is called urea hydrolysis and is explained below. This mechanism allows the H. pylori bacteria to enter the stomach and make their way to the “safe” area – the protective mucous lining of the stomach wall. Once there, the bacterium’s spiral shape helps it burrow through the lining. When the bacterium is in the mucus lining of the stomach, the body’s natural defenses cannot reach it. The immune system will respond to an H. pylori infection by sending white blood cells, killer T cells, and other infection fighting agents, but they cannot reach the infection site as they cannot easily get through stomach lining. They do not go away either, though, and the immune response grows and grows. Polymorphs die, and spill their destructive compounds (superoxide radicals) on the cells of the stomach lining. Extra nutrients are sent to reinforce the white blood cells at the infection site, and the H. pylori bacteria can feed on this.
H. pylori weaken the protective mucous coating of the stomach and duodenum, which allows acid to get through to the sensitive lining beneath. Both the acid and the bacteria irritate the lining. Within a few days of the initial infection, gastritis and perhaps eventually a peptic ulcer will result. Ironically, it may not be H. pylori that causes a peptic ulcer, but the inflammation of the stomach lining; i.e. the response to H. pylori that does so.
Urea Hydrolysis:
Once H. pylori is safely established in the mucus, it is able to fight the stomach acid that does reach it with an enzyme it possesses called urease. Urease converts urea, of which there is an abundant supply in the stomach (from saliva and gastric juices), into bicarbonate and ammonia, which are strong bases. This creates a cloud of acid neutralizing chemicals around the H. pylori, protecting it from the acid in the stomach. The reaction of urea hydrolysis is important for diagnosis of H. pylori by the breath test.
Urea hydrolysis: urea is broken down to ammonia and carbon dioxide
The series of steps – the pathogenic mechanisms – which H. pylori go through when establishing themselves in the stomach are as follows:
1) Attachment – Often initially done with pili (hairlike structures found on the surface of a microorganism, such as a bacterium), other adhesins (surface antigens that bind receptors) may also contribute to an intimate attachment. The secretion system may transfer substances that become receptors, thus further contributing to the attachment process.
2) Toxin production – Toxins increase the secretion of water and electrolytes (enterotoxins) and cause cell death by halting protein synthesis.
3) Cell invasion – H. pylori activates the process of endocytosis (a process of cellular ingestion by which the plasma membrane folds inward to bring substances into the cell) and then destroys the host cell, thus creating tissue damage.
4) Loss of microvilli/villi – The substances secreted into the host cell during the ‘Cell Invasion’ step cause the rearrangement of the actin filaments, resulting in a loss of the microvilli (tiny hairlike structures that project from the surface of certain epithelial layers of the body’s internal organs).
What Causes Ulcers?
Ulcers occur when there is a break down in the mucous protecting layer of your stomach that allows the gastric (stomach) acid and digestive enzymes to attack and aggravate the actual stomach muscle. Helicobacter pylori contribute to this breakdown by living in the mucosa of the stomach and thus increase the chances of a break down in the mucosa lining. Stress and diet can irritate an ulcer, but do not cause it.
What is Peptic Ulcer Disease?
A peptic ulcer is a sore on the lining of the stomach or duodenum, which is the beginning of the small intestine. One cause of peptic ulcers is bacterial infection, but some ulcers are caused by long-term use of non-steroidal anti-inflammatory agents (NSAIDs), like aspirin and ibuprofen. In a few cases, cancerous tumors in the stomach or pancreas can cause ulcers. Peptic ulcers are not caused by stress or eating spicy food.
Peptic ulcer disease has been considered to be a chronic gastrointestinal illness with low mortality but with frequent clinical flare-ups. In the United States population alone, the lifetime prevalence of peptic ulcer disease is about one in ten.
How Common is Infection?
H. pylori infection is common in the United States. About 20% of people under 40 years old and half of those over 60 years have it. Most infected people, however, do not develop ulcers. Why H. pylori do not cause ulcers in every infected person is not known. Most likely, infection depends on characteristics of the infected person, the type of H. pylori, and other factors yet to be discovered.
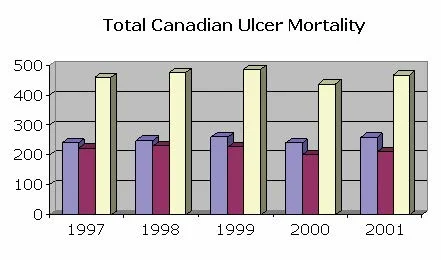
Research has shown that the bacterium, Helicobacter pylori, causes at least 75 % of stomach ulcers and two types of stomach cancer. About 5 million people in the US have peptic ulcer disease and 2.5 million new cases of H. pylori bacteria infections occur each year. Approximately 25 million Americans suffer from peptic ulcer disease at some point in their lifetime. Each year, there are 500,000 to 850,000 new cases of peptic ulcer disease and more than one million ulcer-related hospitalizations. The following graphs outline the peptic ulcer mortality and morbidity statistics for both Canada and the U.S (1997-2001 data). An interesting trend to note is that, in Canada, males tend to experience higher ulcer morbidity and mortality, as compared to females. However, in the U.S, that trend seems to be reversed, with females experiencing higher ulcer morbidity and mortality.
Graph 1: Total discharges from Canadian day surgery and acute care facilities due to digestive ulcers*
Source: Canadian Institute of Health Information (CIHI) http://www.cihi.ca/
*NOTE: Ulcer morbidities were collected from the Canadian Institute of Health Information, by province and by gender. In some provinces, the number of illnesses due to certain digestive ulcers was below 5 and, for privacy protection, the exact numbers were not reported. Therefore, the total Canadian ulcer morbidities represent averaged data. Also, total morbidity was calculated by adding discharges from both, Provincial day surgery and acute care facilities. However, some provinces only reported acute care statistics. Therefore, total reported Canadian morbidities represent lower than actual cases.
Graph 2: Total Canadian deaths due to digestive ulcers
Source: Statistics Canada: Vital Statistics Death Database (Health Statistics)
Graph 3: Total discharges from U.S day surgery and acute care facilities due to digestive ulcers.
** Numbers in thousands
Source: Centers for Disease Control and Prevention (CDC) www.cdc.gov
Graph 4: Total U.S. deaths due to digestive ulcers
Source: Centers for Disease Control and Prevention (CDC) www.cdc.gov
What Are the Symptoms of an H. Pylori Infection?
The recognition of Helicobacter pylori as the major causative agent of chronic gastritis (persistant inflammation of the mucous membreane of the stomach), gastric ulcer disease, and stomach cancer has spawned intensive research on the pathophysiology and epidemiology of this organism.
Abdominal discomfort is the most common symptom. This discomfort usually is a dull, gnawing ache that comes and goes for several days or weeks. It usually occurs 2 to 3 hours after a meal, in the middle of the night (when the stomach is empty), and is relieved by eating, drinking milk or taking antacid medications. Other symptoms include: heartburn, increased burping, weight loss, bloating and burping, and less common symptoms include: poor appetite, nausea and vomiting. It is also important to realize that some people will experience very mild symptoms or sometimes they may not experience any pain or symptoms at all.
If you suspect that you have an ulcer and experience any of the following symptoms, a doctor should be called right away.
- Sharp, sudden, persistent stomach pain
- Bloody or black stools
- Bloody vomit or vomit that looks like coffee grounds
The symptoms just mentioned could be signs of a serious problem, such as:
- Perforation – when the ulcer burrows through the stomach or duodenal wall.
- Bleeding – when acid or the ulcer breaks a blood vessel.
- Obstruction – when the ulcer blocks the path of food trying to leave the stomach.
How Long do the Symptoms Last?
Most people recover from their symptoms within 2-3 weeks after starting antibiotic therapy. Severe symptoms associated with serious ulcer-related problems may take longer to heal.
What Illnesses do H. Pylori Cause?
H. pylori have been associated with many different diseases, including: duodenal ulcers, gastric ulcers, stomach cancer and non-ulcer dyspepsia (indigestion). H. pylori infections have also been linked with causing chronic active, chronic persistent and atrophic gastritis (inflammation of the stomach) in adults and children. Infected persons have a two to six-fold increased risk of developing gastric (stomach) cancer and mucosal-associated-lymphoid-type (MALT) lymphoma (any of various malignant tumors that arise in the lymph nodes or other lymphoid tissue) compared with their uninfected equivalents.
If an ulcer does cause bleeding, prolonged bleeding may cause anemia leading to weakness and fatigue. If bleeding is heavy, hematemesis (the vomiting of blood), hematochezia (the passage of feces containing blood), or melena (a condition marked by black, tarry stool or vomit composed largely of blood) may occur.
How is an H. Pylori Infection Diagnosed?
If an ulcer is found, the doctor will test the patient for H. pylori. This test is important because treatment for an ulcer caused by H. pylori is different from that for an ulcer caused by NSAIDs (Non-Steroidal Anti-Inflammatory Drugs).
An H. pylori infection is diagnosed through blood, breath, stool, and tissue tests, with blood tests being the most common. These four tests are described in detail below.
Blood Tests
Blood tests will identify a Helicobacter pylori infection by detecting the presence of the antibodies that stick to the H. pylori bacteria. If the tests are positive (i.e. the antibodies are present) the bacteria is either currently present, or was present in the recent past (within the past three years).
Carbon-14-urea and Carbon 13-urea Breath Tests
Urea breath tests are an effective diagnostic method for H. pylori and are quicker and simpler to perform than an endoscopy. By drinking a urea solution that contains a special carbon atom, the presence of the bacteria can be determined. If H. pylori are present, they will break down the urea in the solution, thus releasing the carbon. The blood carries the carbon to the lungs, where the patient exhales it. The breath test is 96 percent to 98 percent accurate and can also be used after treatment to see whether it worked.
The C14-urea breath test – A capsule or water containing one microCurie of C14-urea is consumed before a breath sample is provided. This is usually done by blowing up a small balloon or blowing bubbles in a small bottle of collection liquid. Samples of breath are taken between 10 and 20 minutes after the capsule is given. The C14-urea contains a tiny amount of radioactive material which passes out of your body in a day or so in the urine and breath. The amount of radioactive exposure from the test is less than you will normally receive in one day from nature.
The C13-urea breath test – A baseline breath sample is collected by blowing into a bag or tube before eating a small, high calorie, meal. A solution of Carbon-13-urea in water is then drunk before breath samples are taken at twenty, forty and sixty minute-intervals. If H. pylori are present in the stomach, the C13-urea will be broken down and C13 will appear in the breath sample.
Both of these tests may be diagrammed as follows:
Stool Tests
Stool tests may be used to detect an H. pylori infection in a patient’s fecal matter. Studies have shown that this test, called the Helicobacter pylori stool antigen (HpSA) test, is accurate for diagnosing H. pylori. A positive test (i.e. a test that suggests an H. pylori infection), is when antigens, substances that when introduced into the body stimulates the production of an antibody, are found in the fecal matter. The antigens in this case would be the H. pylori bacteria cells.
Endoscopy
An endoscopy diagnoses an H. pylori infection by allowing tissue samples of the stomach and duodenum to be taken for testing. A thin, narrow, flexible, lighted tube with a tiny camera on the end is eased into the mouth and down the throat to the stomach and duodenum. Through this tube (the endoscope), the doctor can examine the lining of the esophagus (food pipe), stomach and duodenum. The endoscope can be used to take photos of ulcers or to remove a tiny piece of tissue to view under a microscope. The removal of tissue samples for observation is a process called a biopsy, and this can be used to check for the presence of H. pylori. Once a biopsy has been obtained, it can be examined by three different types of tests:
- The rapid urease test that detects the enzyme urease, which is produced by H. pylori.
- A histology test that allows the doctor to find and examine the actual bacteria.
- A culture test that involves allowing H. pylori to grow in the tissue sample.
In diagnosing H. pylori, blood, breath, and stool tests are often done before tissue tests (endoscopy) because they are less invasive. However, blood tests are not used to detect H. pylori following treatment because a patient’s blood can show positive results even after H. pylori bacteria have been eliminated. To decide what the best treatment for H. pylori is, it may be necessary to do an endoscopy and take a biopsy (a small piece of tissue) from the lining of the stomach. This allows the sample of H. pylori to be grown in a laboratory in order to determine what antibiotic treatment to use.
How should an H. Pylori Infection be Treated?
Before 1982, when this bacterium was discovered, spicy food, acid, stress, and lifestyle were considered the major causes of ulcers. The majority of patients were given long-term medications, such as H2 blockers, and more recently, proton pump inhibitors, without a chance for permanent cure. These medications relieve ulcer-related symptoms, heal gastric mucosal inflammation, and may heal the ulcer, but they do NOT treat the infection. When acid suppression is removed, the majority of ulcers, particularly those caused by H. pylori, recur. Since we now know that most ulcers are caused by H. pylori, appropriate antibiotic regimens can successfully eradicate the infection in most patients, with complete resolution of mucosal inflammation and a minimal chance for recurrence of ulcers.
Therapy for H. pylori infection consists of 10 days to 2 weeks of one or two effective antibiotics, such as amoxicillin, tetracycline (not to be used for children <12 yrs.), metronidazole, or clarithromycin, plus either ranitidine bismuth citrate, bismuth subsalicylate, or a proton pump inhibitor. Acid suppression by the H2 blocker or proton pump inhibitor in conjunction with the antibiotics helps alleviate ulcer-related symptoms (i.e., abdominal pain, nausea), helps heal gastric mucosal inflammation, and may enhance efficacy of the antibiotics against H. pylori at the gastric mucosal surface. Antibiotic resistance and patient noncompliance are the two major reasons for treatment failure. Overall, triple therapy regimens have shown better eradication rates than dual therapy. Longer length of treatment (14 days versus 10 days) results in better eradication rates.
Current data suggest that persistent infection with Helicobacter pylori may account for the high recurrence rates and the chronicity of peptic ulcer disease. Thus, because of the presence of this organism in ulcers, conventional treatment of peptic ulcer disease has to be altered. At the present time, there is no generally accepted, safe and effective therapy for H. pylori infections. Several clinical trials, using a single antibiotic or even two antibiotics, have found these therapies to be ineffective in eradicating the infection. Worldwide, several large clinical studies are under way to evaluate the best treatment for H. pylori infection.
Of great clinical importance are the recently published epidemiologic data which show a link of H. pylori infection to gastric cancer. In several population studies, there is a significantly higher rate of H. pylori infection among those who had gastric cancer. These findings would strongly strengthen the position that the treatment of H. pylori positive disease should be undertaken and may be chemopreventive for the prevention of gastric malignancy.
Ulcers caused by H. pylori can usually be cured with a one or two week course of antibiotics. Some medicines may cause side effects like nausea; diarrhea; or a black tongue and stools. Possible complications may include a tear in the stomach lining, peritonitis, excessive bleeding, an obstruction in the small intestine, chronic ulcers, and even stomach cancer.
Treatment usually involves a combination of antibiotics, acid suppressors, and stomach protectors. Antibiotic regimens recommended for patients may differ across regions of the world because different areas have begun to show resistance to particular antibiotics.
H. pylori peptic ulcers are treated with drugs that kill the bacteria, reduce stomach acid, and protect the stomach lining. Antibiotics are used to kill the bacteria. Two types of acid suppressing drugs might be used: H2 blockers and proton pump inhibitors.
H2 blockers work by blocking histamine, which stimulates acid secretion. They help reduce ulcer pain after a few weeks. Proton pump inhibitors suppress acid production by halting the mechanism that pumps the acid into the stomach. H2 blockers and proton pump inhibitors have been prescribed alone for years as treatments for ulcers. But used alone, these drugs do not eradicate H. pylori and therefore do not cure H. pylori-related ulcers. Bismuth subsalicylate, a component of Pepto-Bismol, is used to protect the stomach lining from acid. It also kills H. pylori.
The use of only one medication to treat H. pylori is not recommended. At this time, the most proven effective treatment is a 2-week course of treatment called triple therapy. It involves taking two antibiotics to kill the bacteria and either an acid suppressor or stomach-lining shield. Two-week triple therapy reduces ulcer symptoms, kills the bacteria, and prevents ulcer recurrence in more than 90 percent of patients.
Unfortunately, patients may find triple therapy complicated because it involves taking as many as 20 pills a day. Also, the antibiotics used in triple therapy may cause mild side effects such as nausea, vomiting, diarrhea, dark stools, metallic taste in the mouth, dizziness, headache, and yeast infections in women. (Most side effects can be treated with medication withdrawal.) Nevertheless, recent studies show that 2 weeks of triple therapy is ideal.
Early results of studies in other countries suggest that 1 week of triple therapy may be as effective as the 2-week therapy, with fewer side effects. Another option is 2 weeks of dual therapy. Dual therapy involves two drugs: an antibiotic and an acid suppressor. It is not as effective as triple therapy.
Two weeks of quadruple therapy, which uses two antibiotics, an acid suppressor, and a stomach-lining shield, looks promising in research studies. It is also called bismuth triple therapy. In addition, proper antibiotic treatment can completely eradicate the organism, with little chance of its reoccurrence. Treatment of asymptomatic patients with H. pylori infections isn’t warranted unless there is a history of gastric cancer or chronic H. pylori infections in the family.
Drugs Used to Treat H. pylori Peptic Ulcers
For further treatment options and resources, see the following website: www.helico.com, and click on the treatment link.
- Antibiotics: metronidazole, tetracycline, clarithromycin, amoxicillin
- H2 blockers: cimetidine, ranitidine, famotidine, nizatidine
- Proton pump inhibitors: omeprazole, lansoprazole, rabeprazole, esomeprazole, pantoprozole
- Stomach-lining protector: bismuth subsalicylate
Are There Any Long-term Consequences?
The health risk for people infected with H. pylori is very high, about 1 in 5 people will get peptic ulcer disease, about 1 in 200 people will get gastric adenocarcinoma (a malignant tumor originating in the glandular tissue of the stomach), and about 16,000 people die each year in the US as a result of complications from peptic ulcer disease (PUD). Each year in the US nearly 23,000 new cases of gastric adenocarcinoma are diagnosed, and about 13,500 people die from this disease. Gastric cancer has a 5-year survival rate of only about 12%.
Recent studies have shown an association between long-term infection with H. pylori and the development of gastric cancer. Gastric cancer is the second most common cancer worldwide; it is most common in countries such as Colombia and China, where H. pylori infects over half the population in early childhood. In the United States, where H. pylori is less common in young people, gastric cancer rates have decreased since the 1930s Research has shown that the bacteria, Helicobacter pylori, cause at least 75% of stomach ulcers and two types of stomach cancer. About 5 million people in the US have peptic ulcer disease and 2.5 million new cases of H. pylori bacteria infections occur each year. The health risk for people infected with H. pylori is very high, about 1 in 5 people will get peptic ulcer disease, about 1 in 200 people will get gastric adenocarcinoma, and about 16,000 people die each year in the US as a result of complications from peptic ulcer disease (PUD). Each year in the US nearly 23,000 new cases of gastric adenocarcinoma are diagnosed, and about 13,500 people die from this disease. Gastric cancer has a 5-year survival rate of only about 12%.
How do I Get Infected with Helicobacter Pylori? How do the Bacteria Spread?
H. pylori are believed to be transmitted orally. Many researchers think that H. pylori is transmitted orally by means of fecal matter through the ingestion of waste tainted food or water. In addition, it is possible that H. pylori could be transmitted from the stomach to the mouth through gastro-esophagal reflux (in which a small amount of the stomach’s contents is involuntarily forced up the esophagus) or belching, common symptoms of gastritis. The bacterium could then be transmitted through oral contact.
It is not known how the H. pylori bacteria are transmitted or why some patients become symptomatic while others do not. Some epidemiological evidence supports the hypothesis of direct transmission and other studies implicate a water-borne transmission route. The bacteria are most likely spread from person to person through fecal-oral or oral-oral routes. Possible environmental reservoirs include contaminated water sources. Iatrogenic spread through contaminated endoscopes has been documented but can be prevented by proper cleaning of equipment.
How is H. Pylori Infection Spread?
Of all things that are unsure, it is known that an H. pylori infection is:
- Usually acquired in childhood
- More prevalent among African-Americans, Hispanics, lower socioeconomic groups, and older adults (in the U.S.). Half of all adults over the age of 50 in the U.S. have an H. pylori infection.
Because of good sanitation practices and standards of living, there are fewer children in the United States with H. pylori infection than previously recorded, yet about two-thirds of the world’s population remains infected with H. pylori.
The most probable way that the bacterium is spread is through the fecal-oral or oral-oral route. (Bacteria from an infected person end up in the food or water of an uninfected person through improper water and sewage treatment or improper food handling.)
Researchers are not certain how people contract H. pylori, but they think it may be through contact with food or water sources that are contaminated with feces. Risk increases with a family history of ulcers; exposure to contaminated sources; poor sanitation; and crowded living conditions. H. pylori has been found in the saliva of some infected people, so the bacteria may also spread through mouth-to-mouth contact such as kissing.
How Can I Prevent Getting Infected with H. Pylori?
Since the source of H. pylori is not yet known, it is difficult to list what should be avoided in order to prevent infection. In general, people should maintain proper hygiene by washing their hands thoroughly, eating food that has been properly prepared, and to drinking water from a safe, clean source.
How do I Prevent Spreading it to Others?
As of present, there is not a specific method of preventing the spread of Helicobacter pylori. The CDC, with partners in other government agencies, academic institutions, and industry, is currently conducting a national education campaign to increase the awareness of the link between H. pylori and stomach / duodenal ulcers. Research and studies are also being done to determine the routes of transmission and possible prevention measures, and to establish an antimicrobial resistance surveillance system to monitor the changes in resistance among H. pylori strains in the United States.
How Prevalent is Helicobacter in Surface Water/Well Water?
The existence of environmental reservoirs has been suggested, and epidemiological studies indicate that water can be a source of H. pylori infection. Preliminary research regarding the occurrence of H. pylori in surface water and ground water has been conducted and data indicates that Helicobacter pylori are frequently present in surface and groundwater. Recent research at Penn State University - Harrisburg has shown a statistically significant link between people who have peptic ulcer disease and H. pylori bacteria contamination in their private well. Researchers found that a high percentage of wells (85%) that have coliform bacteria also have the H. pylori bacteria and that 65% of private well water samples and 75% of surface water samples contained the H. pylori bacteria.
The USEPA Office of Ground Water and Drinking Water has recently included H. pylori on the Contaminant Candidate List (CCL) – a list that designates contaminants which are not currently regulated under the national primary drinking water regulation (NPDWR), but which are known or anticipated to occur in public water systems. These contaminants may evetually require regulations under the Safe Drinking Water Act (SDWA).
How Can We Protect Our Water Supplies?
There is a need for a systematic survey of environmental and potable waters for the presence of Helicobacter pylori, as its presence in source or finished water has profound public health and epidemiological implications. The potential presence of the organism in source water necessitates the documentation of treatment and disinfection procedures to prevent infection of drinking water consumers.
Is My Water Safe? How Can I Tell?
The water industry has usually relied on coliform bacteria, a bacterial indicator, to evaluate the safety of source waters. Unfortunately, H. pylori have commonly been found in waters where coliform indicators were absent, thus making its detection in water sources very difficult.
The high prevalence of H. pylori in the limited number of monitoring efforts to date indicate an urgent need for the development of rapid, specific and reliable detection methods in order to evaluate the potential impact of the waterborne role in H. pylori infections.
What Are Some Ways I Can Treat My Water to Ensure its Safety?
H. pylori are sensitive to conventional methods of water treatment (i.e., chlorination) and thus aren’t thought to be a problem with properly treated water supplies. Studies using ultraviolet light or ozone haven’t been done in great abundance and thus their effectiveness is not clear.
Identifying H. pylori organisms in environmental samples is complicated by the fact that viable, coccoid forms of the bacterium may not be culturable in a laboratory setting. Polymerase chain reaction (PCR) amplification of the 16S ribosomal gene sequences contained within the bacteria permit the sensitive and specific detection of H. pylori in environmental water samples resulting in the identification of water sources contributing to the risk of human H. pylori infection.
Did you know that our Operation Water Health program is available free of charge to teachers worldwide and provides the teachers with all of the lesson plans and information they need to teach students about what safe drinking water is, what unsafe drinking water is, and what health problems can be caused by unsafe drinking water? Please help us to keep our Operation Water Health program up-to-date! Please chip in $5 or donate $20 or more and receive an Official Donation Receipt for Income Tax Purposes.